Mrs R is a 55 year old lady who presented with a three year history of lateral foot pain and intermittent instability. This was initially treated with osteopathy, who astutely diagnosed peroneal tendinopathy and commenced Mrs R on a comprehensive rehabilitation program. She initially did very well but unfortunately the pain recurred and she was referred to Dr Touzell for an opinion.
On examination, Mrs R had normal hindfoot alignment, without a cavovarus foot type that can predispose patients to peroneal tendon pathology. She had point tenderness to palpation over her lateral ankle in the area of the peroneal tendons, and ankle eversion in both plantarflexion and plantargrade was painful. Her peroneal tendon function was limited by pain. There was no evidence of ankle instability.
An initial ultrasound had reported a lipoma which was a bit unusual, so an x-ray and MRI scan were performed (see below):


The x-ray and MRI scan demonstrated a hypertrophied peroneal tubercle, inflamed os peroneum and tendinopathy of the peroneus brevis tendon.
It was therefore suggested to trial an injection of local anaesthetic and steroid around the os peroneum, counselling Mrs R about the 1% risk of tendon rupture.
Combined with an ongoing rehabilitation program, the steroid injection gave Mrs R approximately twelve months of relief. However the pain recurred, including significant night pain, and she was ready to consider surgical intervention.
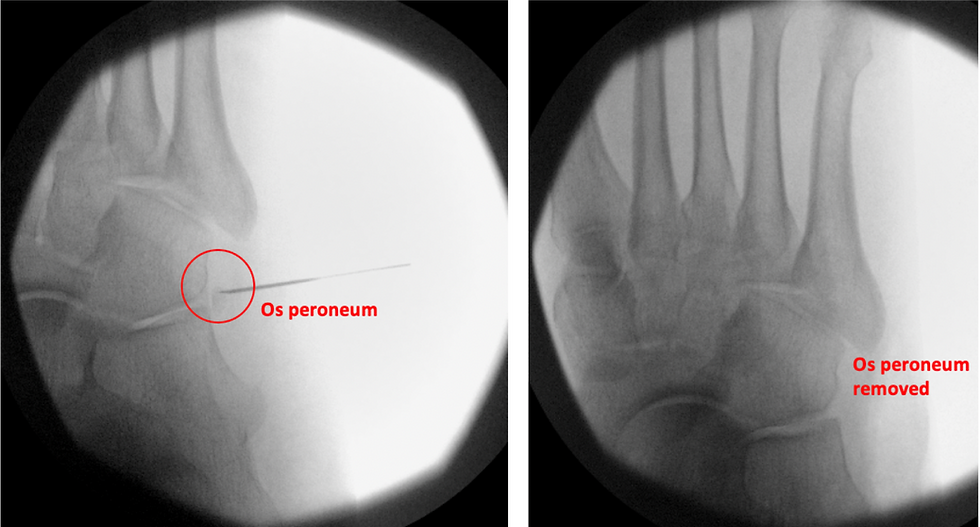
The risks and benefits of excision of the os peroneum, combined with a debridement of the peroneal tendons and possible peroneus longus to brevis transfer if required were therefore discussed. Intra-operatively, it was noted the tendon of peroneus longus was extremely degenerate and frayed, so a peroneus longus to brevis transfer was performed. The os peroneum was successfully excised, and the hypertrophied peroneal tubercle removed (see intra-operative imaging below):
Mrs R was non weight bearing for two weeks, then comfortably started weight bearing in an ankle brace two weeks following her surgery. She started some simple seated calf raises, and was able to progress to single leg calf raises and return to walking independently six weeks following surgery. Six months down the track, she still has some stiffness in her ankle. However, her night pain has resolved completely, she is walking 10-15km per day and no longer has ankle instability.
Key Learning Points:
An os peroneum is a normal variant in 9-20% of the population. However, in some instances this accessory bone can become inflamed in the setting of ankle instability or direct trauma.
Painful os peroneum syndrome is associated with attrition of the peroneus longus tendon as it passes into the sole of the foot causing intrasubstance tears, swelling and (rarely) complete rupture of the tendon.
MRI is the most appropriate imaging modality to assess the peroneal tendons, lateral ligaments and integrity of the os peroneum.
A rehabilitation program focusing on calf strength and peroneal tendon strengthening, possibly combined with an ultrasound guided steroid injection in and around the os peroneum, is reasonable first-line treatment.
Surgical excision and peroneal tendon debridement, repair and/or transfer is an option for cases not amendable to non-operative treatment.
All cases and clinical photographs have been shared following discussion and written permission from the patient and/or guardian.
